By 2050, More People Will Die from Antibiotic resistance Than from Cancer. Professor Refers to It as A Medical Climate Crisis.

Dag Berild is Professor and Chief Physician at Oslo Met University and Oslo University Hospital. Photo: Stortinget
It is not your typical Arctic conference topic; however, during The Northern Dimension in Bodø this week it nevertheless received much attention. – Resistance against antibiotics is the climate crisis of medicine, says Chief Physician and Professor Dag Berild.
Antibiotics do not only help your sore throat in winter, it saves millions of lives around the globe every year. One out of five cancer patients depend on antibiotics. Some forms of cancer simply cannot be treated without. And even simple surgical procedures could be fatal if we did not have medicines to knock out infections.
However, if we are to believe the English economist Jim O’Neill, the fact is that the number of deaths from resistance to antibiotics will surpass the number of deaths from cancer by 2050 – if nothing is done about it. O’Neill was asked by the British government to investigate the economic consequences that would come if we do not take antibiotic resistance seriously.
Over-consumption
Antibiotic resistance means that antibiotics no longer kill bacteria. The reason why antibiotic resistance occurs is – simply explained – that we use too much of it.
- What happens when we prescribe antibiotics is that we kill the pathogenic bacteria. However, in a bacteria population of for instance 10 million, there will always be some of the bacteria that are resistant. When we kill the antibiotics-sensitive bacteria, the resistant bacteria get the opportunity to reproduce. And it goes fast, as they only have a generation time of 15 to 20 minutes. After some time, the antibiotics-sensitive bacteria will be replaced by resistant mutations, explains Dag Berild, Professor and Chief Physician at Oslo University Hospital (OUS) and Oslo Met.
So why not just make new medicines? Because it no longer pays off. It is much cheaper and more profitable to produce medicines that are used every day, such as painkillers and tranquilizers, than to produce medicine that is to be used as little as possible.
Making medicines the use of which we have to reduce does not make anyone rich
- Making medicines the use of which we have to reduce does not make anyone rich. And the medical industry has stopped taking an interest in developing new antibiotics. It has been 30 years since the most recent antibiotic hit the market. 16 years ago, there were 16 companies producing antibiotics. Today, only four remain and that is despite the World Health Organization’s stating that antibiotic resistance is one of the greatest threats the world is facing, he says.
Resistance increases. Production drops. However, it is not human use of antibiotics that is the biggest problem. People only account for some 25 percent of antibiotics used in the world. The rest is used as growth promoters for animals by the food industry.
- Using antibiotics in the food industry is prohibited in the EU, however, it is permitted in the USA, India and China. In the USA alone, 70 percent of antibiotics consumption goes to animals. And the resistant bacteria are contagious from animals to humans, he warns.
Penicillin was discovered by Alexander Fleming in 1941 and it is the biggest medical invention of our time. However, Fleming himself warned only a few years later that over-consumption would lead to resistance.
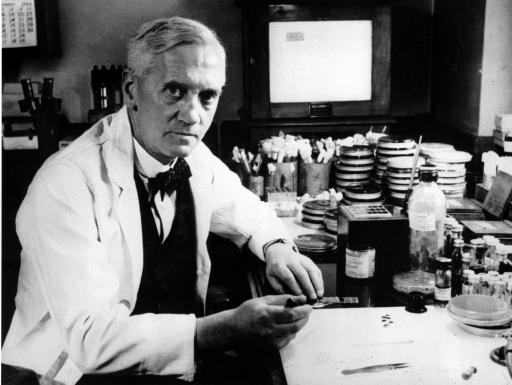
Alexander Fleming discovered penicillin in 1941 and warned early about resistance. Photo: Lenny Flank/Flickr
Before the discovery of penicillin, you had only 60 percent chance of surviving a serious bout of pneumonia if you were between the ages of 50 and 60, according to a study conducted on the Boston population in the 1930s. Today, the likelihood of dying is only a very few percent.
70 years back in time
- What happens now, is that the world is about to be put 70 years back in time. It is also an ethical question. We use up antibiotics so that there is none left for our children and grandchildren. And the longer we delay in acting, the more expensive it will be. The more we use, the worse it gets. Bacteria develop resistance faster than we can make new medicine, Berild says.
He has worked on antibiotics and resistance for 30 years and refers to the World Health Organization’s referring to antibiotic resistance as the biggest threat against human health.
- It is the climate crisis of medicine. Antibiotics is a limited resource and resistance is man-made. By 2050, more people will die from resistance than from cancer. Modern medicine, such as transplants and advanced surgical procedures will be impossible without working antibiotics.
Antibiotic resistance will potentially lead to an economic crisis like the one we had in 2008
Dr Berild uses the STD gonorrhea as an illustration of the problem.
- Gonorrhea is a ticking bomb. Sex has come to stay; we have to admit as much. However, we see that in some places, a fully resistant gonorrhea has developed. And chronic gonorrhea makes it easier to contracts other STDs, such as HIV.
A lasting financial crisis
He also warns against the economic consequences.
- Antibiotic resistance will potentially lead to an economic crisis like the one we had in 2008, however, the difference is that this one will last. Resistance will lead to a finance crisis and radically affect the world economy.
The World Bank also shares Dr Berild’s worries and writes in a statement that: “(…) if governments cannot act now, the world will have to pay a lot more in the future to manage the escalating effect of uncontrolled antibiotic resistance. Securing such economic commitments will require solid management (…)”
Or in the words of the Jim O’Neill report: “The costs when it comes to lost global production between now and 2050 would be an enormous 100 billion dollars if we do not act.”
Requires leadership
However, the chief physician stresses that the game is not completely lost. He has conducted a series of tests, both nationally as well as internationally, where the use of antibiotics was dramatically cut, without other effects than cutting costs. A similar test has been conducted in St. Petersburg too, with similar results.
- However, that requires three things: Leadership, leadership and leadership. We must have the political will to do so. Will from hospital management, as well as national and global guidelines doctors must reduce use of antibiotics, the farming industry must stop using antibiotics to get raise fat chicken and politicians must take responsibility. We should also have digital support tools and solid vaccination programs, in addition to continuing our work to make sure the world’s population has clean water and good sewage systems, he says and stresses:
- We cannot win against the bacteria, but we can lower the consequences.
Berild praises Norwegian veterinarians and farmers who are those of their kind who use the least antibiotics in the whole world.
Norwegian authorities have an action plan with the target of reducing use of antibiotics by 30 percent during the 2012-2020 period, and they are on schedule.
Wants to in-source production
- It is also decisive for us to stop thinking profits when it comes to production of antibiotics, Berild argues, and says we should in-source production.
- Antibiotics is not a regular commodity, but a shared good. Today, antibiotics are produced in the East and we experience problems with deliveries as well as false products. This is about patient security and production of antibiotics should take place in Norway or Scandinavia he says and closes:
- Like we say about the climate crisis; we should think global and act local.
Nordic-Russian cooperation against resistance
One of the partnerships of The Northern Dimension is a program cooperation between Russia and the Nordic countries focusing exactly on reducing antibiotic resistance. The program, which commenced January 2019, is funded by a.o. the Nordic Council of Ministers.

Dmitry TItkov chairs the Nordic-Russian partnership for fighting antibiotic resistance. Photo: Stortinget
- Antibiotic resistance is a global and increasing problem and no nation can fight it alone. Nor is it a problem limited to one sector; only 20-25 percent of consumption is for humans, the rest is found in farming, says Dmitry Titkov, who is project manager and works at the THL Institute, the Finnish institute of health and welfare.
People move a lot, shop a lot, tourism increases, as does medical tourism.
- This is why it is extra important to form cooperative networks, more committees and cooperation platforms.
Russia is one of the countries that has taken recent measures on a political level to solve the problem of antibiotic resistance. In 2017, a national strategy was adopted. And in 2018, an action plan was introduced. And then there’s the partnership, founded this year.
Gather and disseminate knowledge
The goal of the project is to prevent antibiotic resistance from spreading, establish coordinated strategies based on modern and updated information as well as comparative data that have a scientific foundation.
- In our project, we will form the foundation for mutually beneficial cooperation that will benefit the Nordic countries and Northwestern Russia. we are to ensure possibilities for exchanging information and experience and implementation of national strategies. Through new cooperation initiatives we hope that it will be easier with people-to-people contact between the West and Russia, Titkov says.
The Russian strategy is primarily about informing the population about the risks of resistance and to train health personnel. In addition, monitoring will be coordinated and experiences about best practices shared.

Ülla-Karin Nurm is Director of the Northern Dimension’s partnership for health and welfare. Photo: Stortinget
- Personally, I was surprised when I learned how active Russian specialists are about fighting this problem. Antibiotic resistance is in many ways new to us and there is no research on it until now. What we already are learning is that the dose is too large and the cure too long when relating it to the disease it is to cure. However, we also see that there is a keen interest in learning and a large turnout when we organize seminars, Titkov says.
Resistance does not care about borders
Ülla-Karin Nurm is Director of the Northern Dimension’s partnership for health and welfare. She encourages even more cross-border cooperation.
- The threat we face with antibiotic resistance does not care about national borders. We therefore have to cooperate more, and it also takes political effort. We need to asses the problems both nationally as well as internationally, and comparable data must be made available for both health personnel as well as decision-makers.
The Northern Dimension Antibiotic Resistance Study (NoDARS) is a partially EU funded project hat has covered six year and six countries. The project has had two phases, one of which focused on the level of E-coli in patients with UTI’s, and the other on how infection spreads in society.
- Common infections, such as UTI’s, will be more difficult to cure if resistance increases. Taking pills at home will no longer be enough, you may have to go to a hospital to get intravenous antibiotics. The study gave us new knowledge about resistance among patients who usually do not get it, such as women and outpatients, a group that one has not investigated much until now, Nurm says, referring to the project as groundbreaking.

Bente Stein Mathisen chairs the Nordic Council Welfare Committee and represents the Conservative Party in the Norwegian parliament. Photo: Stortinget
The goal is to use the study to improve existing guidelines and provide a knowledge foundation for political measures.
One of the most important issues
Bente Stein Mathisen, who chairs the Nordic Council Welfare Committee and represents the Conservative Party in the Norwegian parliament, refers to antibiotic resistance as “one of the most important issues we should raise awareness about and gain more knowledge of”.
- That is why I am very happy that the issue has received a key role on the program of the Northern Dimension during the World Antibiotic Week. The Nordic Council has been engaged with the issue of resistance since 2011 and we want to spearhead further work. We want the Nordic to be a groundbreaking region when it comes to the fight against antibiotic resistance, she says.
It is important that we act. If not, we run the risk of antibiotics killing us before the climate does.
She refers to 12 specific proposals for new Nordic initiatives against resistance. Some of them have been followed up, others are in process in the respective countries.
- A joint Nordic public awareness campaign is one of the most important tools. In order for antibiotics to be effective, they have to be used right and to the least degree possible. If the current development continues, we may approach a situation like the one we were in before the war. It is vital that we do something. If not, we risk that the antibiotics kill us before the climate does.
This article was originally published in Norwegian and has been translated by HNN's Elisabeth Bergquist.

